Tietze Syndrome vs Costochondritis: How to Tell Them Apart

Disclaimer: Please note that the information provided in this article is not intended as a substitute for professional medical advice. Before taking any treatment, it is best recommended to consult a healthcare professional.
Chest pain can be alarming and often raises concerns about heart disease. However, not all chest pain is heart-related.
Tietze syndrome and costochondritis are common non-cardiac causes of acute chest pain, involving inflammation of the cartilage connecting the ribs to the sternum.
Despite their similarities, these conditions have distinct characteristics essential for accurate diagnosis and effective treatment.
This article delves into Tietze syndrome and costochondritis, offering an in-depth comparison to aid patients, healthcare providers, and medical enthusiasts.
By examining their symptoms, causes, diagnostic criteria, and treatment options, we aim to clarify the differences and guide appropriate management strategies.
Understanding these distinctions not only alleviates patient concerns but also enhances clinical outcomes. Join us as we explore the unique features and commonalities of Tietze syndrome and costochondritis.
What is the Tietze Syndrome?
Tietze syndrome involves the inflammation of one or more of the upper ribs' costal cartilages, typically around the second or third ribs (NORD, 2016).
This inflammation causes localized swelling that is usually visible and can be felt during a physical examination.
Unlike costochondritis, which affects multiple sites along the rib cage, Tietze syndrome typically involves a single site of inflammation
Understanding Tietze syndrome's distinct features and effective management strategies is essential for both patients and healthcare providers.
With proper diagnosis and treatment, individuals can achieve relief from symptoms and maintain a good quality of life.
Symptoms
- Swelling - The most distinguishing feature is localized swelling at the costosternal, costochondral, or costovertebral joints. This swelling is usually tender to the touch.
- Pain - Patients often experience sharp, aching, or pressure-like pain at the site of inflammation. The pain can radiate to nearby areas such as the arms, shoulders, and upper back.
- Tenderness - The affected area is typically very tender, and pressure on the swollen region can exacerbate the pain.
These symptoms may vary and can be triggered or worsened by physical activity, deep breathing, or coughing.
Causes and Risk Factors
The exact cause of Tietze syndrome remains unclear, but several factors are believed to contribute to its development:
- Trauma: Physical injury or repetitive strain to the chest area can trigger inflammation.
- Infection: Respiratory infections may lead to inflammation of the costal cartilage.
- Overuse: Activities that involve excessive use of the chest muscles, such as vigorous exercise or heavy lifting can be risk factors.
- Idiopathic: In many cases, no specific cause is identified, making the condition idiopathic.
Tietze syndrome is more commonly seen in younger individuals, typically those under 40 years old, and there is no clear gender predisposition.
Diagnosis
Diagnosing Tietze syndrome relies on a thorough clinical examination and patient history. Key diagnostic steps include:
- Physical Examination - Localized swelling and tenderness at the costal cartilage is a critical diagnostic marker.
- Patient History - A detailed history of symptoms, onset, and potential triggers (such as recent trauma or respiratory infections) helps ensure the accuracy of how tietze syndrome diagnosed.
- Imaging Studies - While not always necessary, imaging techniques like ultrasound, MRI, or X-rays can be used to help diagnose tietze syndrome.
It's important to differentiate Tietze syndrome from other causes of chest pain, such as costochondritis, cardiac conditions, and rib fractures.
Treatment and Management
Managing Tietze syndrome focuses on relieving pain and reducing inflammation. Common treatment approaches include:
- Rest - Avoiding activities that exacerbate symptoms is crucial for recovery.
Pain Management—Over-the-counter analgesics and NSAIDs, such as acetaminophen and ibuprofen, are commonly used to manage pain and inflammation.
Corticosteroid Injections - In cases of severe pain, corticosteroid injections directly into the affected area can provide significant relief.
Physical Therapy - Gentle exercises and physical therapy can help maintain mobility and reduce discomfort.
Heat and Cold Therapy - Applying heat or cold packs to the affected area can alleviate pain and swelling.
The prognosis for Tietze syndrome is generally good.
With appropriate treatment, many patients experience a significant reduction in symptoms.
However, the condition can recur, requiring ongoing management and attention to avoid triggering factors.
Understanding Tietze syndrome's distinct features and effective management strategies is essential for both patients and healthcare providers.
With proper diagnosis and treatment, individuals can achieve relief from symptoms and maintain a good quality of life.
What is Costochondritis?
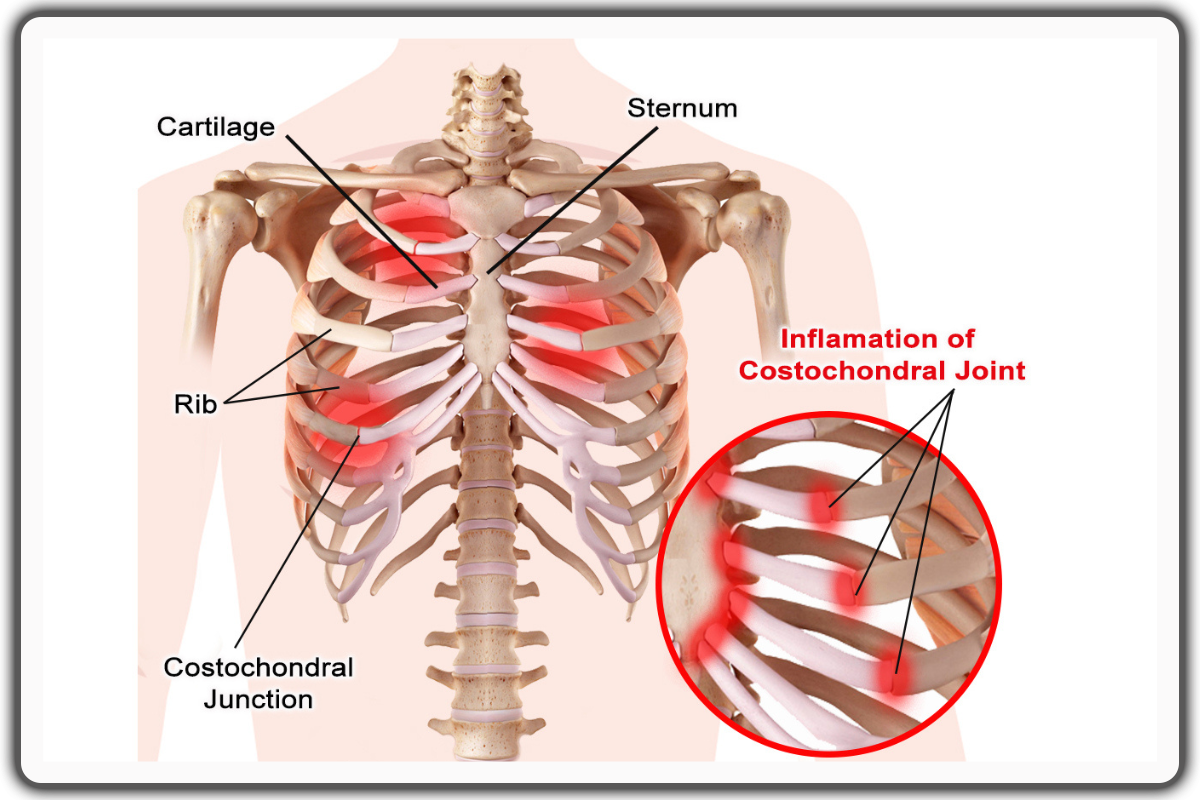
Costochondritis is the inflammation of the costal cartilage, which connects the ribs to the sternum (Proulx & Zryd, 2009).
It is benign but can cause significant discomfort and concern due to its location and the similarity of its symptoms to those of heart-related conditions.
Costochondritis typically presents as localized pain and tenderness at the costosternal, costochondral, or costovertebral joints.
The pain is usually felt in the upper ribs, most commonly affecting the second to fifth ribs.
Unlike Tietze syndrome, there is no visible swelling at the affected site.
Symptoms
- Pain - The primary symptom is chest pain, which may be sharp, aching, or pressure-like.
- The pain is usually localized to one area but can radiate to other parts of the chest or upper abdomen.
- Tenderness - The affected area is tender to touch.
- Pressing on the ribs at the costosternal junction can reproduce the pain.
- No Swelling - Unlike Tietze syndrome, costochondritis does not cause visible or palpable swelling.
Causes and Risk Factors
Potential Causes
- Idiopathic - In many cases, the exact cause of costochondritis is unknown.
- Physical Strain - Activities that involve heavy lifting, strenuous exercise, or repetitive movements can lead to inflammation.
- Infections - Respiratory infections, especially those involving a persistent cough, can contribute to the development of costochondritis.
- Trauma - Direct injury to the chest area can trigger inflammation of the costal cartilage.
Risk Factors and Demographics
- Age - Costochondritis can affect individuals of any age but is more common in adults.
- Activities - People engaged in activities that strain the chest muscles, such as weightlifting or heavy manual labor, are at higher risk.
- Gender - It can affect both men and women, with studies suggesting a higher prevalence in women.
Diagnosis
Diagnosing costochondritis is primarily based on the patient's history and physical examination. Key diagnostic criteria include:
- Localized Pain: Pain that can be reproduced by pressing on the affected area of the chest.
- Absence of Swelling: Lack of visible swelling helps distinguish costochondritis from Tietze syndrome.
Treatment and Management
Common Treatments
The following treatments are best recommended, given that the problem
- Rest: Limiting activities that aggravate the pain is essential.
- NSAIDs: Ibuprofen or naproxen and other Nonsteroidal anti-inflammatory drugs are commonly used to lessen inflammation and pain.
- Physical Therapy: Strengthening exercises and gentle stretching can help alleviate symptoms and improve mobility.
- Heat and Cold Therapy: Applying cold or heat packs to the affected area can help ease the pain and inflammation.
Long-term Management Strategies and Prognosis
For many individuals, costochondritis resolves with conservative treatment. However, in cases of persistent pain, additional strategies may include:
- Corticosteroid Injections - Injections at the site of inflammation can provide relief for severe or chronic pain.
- Avoiding Triggers - Identifying and avoiding activities or movements that exacerbate the condition can help prevent recurrence.
- Lifestyle Modifications - Incorporating regular, moderate exercise and maintaining good posture can relieve strain on the chest.
The prognosis for costochondritis is generally good, with most people experiencing significant improvement over time.
However, individuals who have recurrent episodes require ongoing management and periodic reassessment by a healthcare provider.
Understanding costochondritis and adhering to recommended treatment plans can help patients manage symptoms effectively and maintain a good quality of life.
Comparing Tietze Syndrome and Costochondritis
Tietze syndrome and costochondritis are the major causes of musculoskeletal chest pain. They often cause confusion due to their similar symptoms and the areas they affect.
Both involve inflammation of the costal cartilage at the junction where the ribs meet the sternum, leading to chest pain (Schumann, et. al., 2024)
However, there are several key differences between the two conditions that are important for accurate diagnosis and effective treatment.
Key Similarities
Symptoms and Affected Areas
- Chest Pain: Both conditions present with chest pain, which can range from sharp to dull and may radiate to nearby areas, such as musculoskeletal chest wall pain.
- Tenderness: Tenderness over the costosternal, costochondral, or costovertebral joints is common in both conditions. Palpation of the affected areas usually elicits this tenderness.
- Inflammation: Inflammation of the costal cartilage is the underlying cause of symptoms in both conditions.
Diagnosis
- Clinical Examination: Diagnosis for both conditions relies heavily on clinical examination and patient history.
- The absence of more serious conditions like cardiac issues is crucial.
- Exclusion of Other Causes: Both conditions require the exclusion of other potential causes of chest pain, such as myocardial infarction, pulmonary embolism, or rib fractures.
Key Differences
Presence of Swelling
- Tietze Syndrome: One of the hallmark features of Tietze's syndrome is the presence of visible and palpable swelling at the site of inflammation.
- This swelling is typically localized to the upper ribs, most commonly at the second or third costal cartilage.
- Costochondritis: Costochondritis does not involve visible or palpable swelling.
- The inflammation and tenderness are present without any external signs of swelling.
Age Group Prevalence
- Tietze Syndrome: More commonly affects younger individuals, often those under the age of 40. It is relatively rare compared to costochondritis.
- Costochondritis: Can affect people of any age but is more commonly seen in adults. It is a more frequently encountered condition in clinical practice.
Cause and Risk Factors
- Tietze Syndrome: Often linked to physical trauma, repetitive strain, or upper respiratory infections. However, in many cases, the exact cause remains unknown.
- Costochondritis: Similarly can be caused by physical strain or trauma, but idiopathic cases are more common. Respiratory infections and conditions involving chronic coughing are also contributing factors.
Treatment Approaches
- Tietze Syndrome: Treatment often involves rest, NSAIDs, and corticosteroid injections for severe cases.
- Physical therapy may also be advised to manage symptoms and maintain mobility.
- Costochondritis: Treatment typically includes rest, NSAIDs, and physical therapy.
- Heat and cold therapy are also commonly used to alleviate symptoms. Corticosteroid injections are considered in persistent or severe cases.
Prognosis and Recurrence
- Tietze Syndrome: Generally has a good prognosis with appropriate treatment, but symptoms can recur, requiring ongoing management.
- Costochondritis: Also has a favorable prognosis, with many individuals experiencing significant improvement with conservative treatment.
However, some patients may have recurrent episodes, necessitating long-term management strategies.
Clinical Approach to Differentiation
Diagnostic Criteria
- Swelling Check: The presence or absence of swelling is a critical factor in differentiating between Tietze syndrome and costochondritis.
- Swelling at the costosternal junction points towards Tietze syndrome.
- Patient History: Detailed patient history, including recent activities, trauma, or respiratory infections, helps in identifying potential triggers and distinguishing between the two conditions.
- Physical Examination: Palpation of the anterior chest wall to identify tenderness and any visible swelling aids in diagnosis.
- The response to palpation and the distribution of tenderness can provide important diagnostic clues.
Management Strategies
- Symptom Relief: Both conditions prioritize symptom relief through the use of NSAIDs and rest.
- The application of heat or cold packs can help reduce pain and inflammation.
- Long-term Care: For persistent or recurrent cases, long-term management strategies such as lifestyle modifications, regular exercise, and avoiding activities that strain the chest muscles are recommended.
Conclusion
While Tietze syndrome and costochondritis share several similarities, their key differences lie in the presence of swelling, the prevalence in age groups, and specific triggers.
Accurate diagnosis requires careful clinical examination and patient history.
It ensures that each condition is managed with the most appropriate treatment strategies to provide relief and improve the patient's quality of life.
References
National Organization for Rare Diseases (2016). Tietze Syndrome.
https://rarediseases.org/rare-diseases/tietze-syndrome/
Proulx, A. M., Zryd, T. W. (2009). Costochondritis: Diagnosis and Treatment. Wright State University Boonshoft School of Medicine.
https://www.aafp.org/pubs/afp/issues/2009/0915/p617.pdf
Schumann, J. A., Sood, T., Parente, J. J. (2024). Costochondritis. National Library of Medicine.
https://www.ncbi.nlm.nih.gov/books/NBK532931/
